Coronavirus (COVID-19) Guidance for Ship Operators for the Protection of the Health of Seafarers
Source: International Chamber of Shipping – Version 1.0 – 3 March 2020
1 Introduction
In response to the current coronavirus (COVID-19) outbreak, this Guidance has been produced by the International Chamber of Shipping (ICS) to support all types of ships which operate in international waters. The purpose is to help shipping companies follow advice provided by United Nations agencies including the World Health Organization (WHO), the International Maritime Organization (IMO) and the International Labour Organization (ILO), as well as the European Centre for Disease Prevention and Control (ECDC).
COVID-19 – a virus which can lead to respiratory disease and pneumonia – was first reported in December 2019 in Wuhan, China. More than 90,000 cases have been reported at the time of going to print, including several thousand deaths. While most of these have been concentrated in China, the virus now appears to be spreading globally. No vaccine is currently available, and the focus of health authorities worldwide has been containment of the virus through preventative measures to limit and slow down widespread transmission.
The WHO has declared the outbreak a Public Health Emergency of International Concern under the WHO International Health Regulations (IHR).
This severe public health challenge requires close co-operation between governments and shipping companies engaged in maritime trade, in order to protect the health of seafarers (and passengers) as well as the general public.
ICS is grateful for the support of the following organisations in preparing this Guidance: IMO, ILO, WHO, International Maritime Health Association (IMHA), European Centre for Disease Prevention and Control (ECDC), Mediterranean Shipping Company S.A. (MSC) and Wilhelmsen Ships Service.
2 Port Entry Restrictions
WHO, as at 3rd March 2020, has not currently recommended any international travel or trade restrictions, and according to the IHR (and other international regulations) ships shall not be refused ‘free pratique’ by the IHR state parties for public health reasons, i.e. permission to enter a port, embark or disembark discharge or load cargo or stores. The IHR states Parties may subject granting free pratique to inspection, and, if a source of infection or contamination is found on board, conduct necessary, disinfection, decontamination, disinsection or deratting, or other measures necessary to prevent spread of the infection or contamination.
The WHO IHR can be available at www.who.int/ihr/publications/9789241580496/en/
Nevertheless, many governments have now introduced national and local restrictions including:
• Delayed port clearance;
• Prevention of crew or passengers from embarking or disembarking (preventing shore leave and
crew changes);
• Prevention of discharging or loading cargo or stores, or taking on fuel, water, food and supplies; and
• Imposition of quarantine or refusal of port entry to ships (in extreme cases).
While such measures can severely disrupt maritime traffic – and may well be in breach of the IHR, the Convention on Facilitation of International Maritime Traffic (FAL Convention) and other maritime principles regarding the rights and treatment of seafarers and passengers – the reality is that shipping companies may have little choice but to adhere to these national and local restrictions due to the serious concern about COVID-19 and the potential risk to public health.
However, it is very important for port States to accept all ships (both cargo and passenger), for docking and to disembark suspected cases on board, as it is difficult to treat suspect cases on board and it could endanger others.
If any infection or contamination is found on board visiting ships, port States may take additional measures to prevent spread of the infection or contamination.
Together with flag States, companies and Masters should co-operate with port State authorities to ensure, where appropriate, that:
• Seafarers can be changed;
• Passengers can embark and disembark;
• Shore leave can continue if safe to do so;
• Cargo operations can occur;
• Ships can enter and depart shipyards for repair and survey;
• Stores and supplies can be loaded; and
• Necessary certificates and documentation can be issued.
ILO has advised that during the evolving COVID-19 outbreak, effective protection of the health and safety of seafarers must remain a priority. Under the ILO Maritime Labour Convention (MLC), flag States must ensure all seafarers on ships flying their flag are covered by adequate measures to protect their health and that they have access to prompt and adequate medical care while working on board.
Port States must ensure that any seafarers on board ships in their territory who need immediate medical care are given access to medical facilities on shore.
Wilhelmsen Ships Service has developed an interactive map on current port restrictions which is available at https://wilhelmsen.com/ships-agency/campaigns/coronavirus/coronavirus-map
3 Protective Measures Against COVID-19 for Seafarers
Human-to-human transmission of COVID-19 is understood to occur primarily through droplets from a person with COVID-19, e.g. from coughing and sneezing, landing on objects and surfaces around the person. Other people then catch COVID-19 by touching these objects or surfaces, then touching their eyes, nose or mouth. People can also catch COVID-19 if they breathe in droplets from a person with COVID-19 who coughs, sneezes or breathes out droplets.
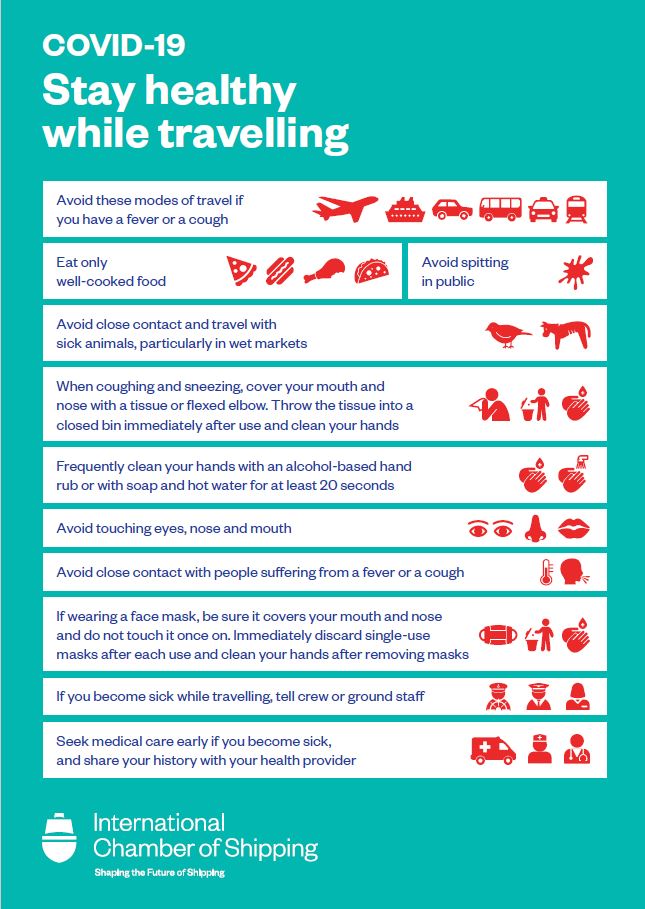
Seafarers (on board ship or on leave) should inform their healthcare providers if they have visited an area where COVID-19 has been reported within the past 14 days, or if they have been in close contact with someone with respiratory symptoms who has been to a place which has COVID-19.
If seafarers have fever, cough or difficulty breathing it is important to seek medical attention promptly.
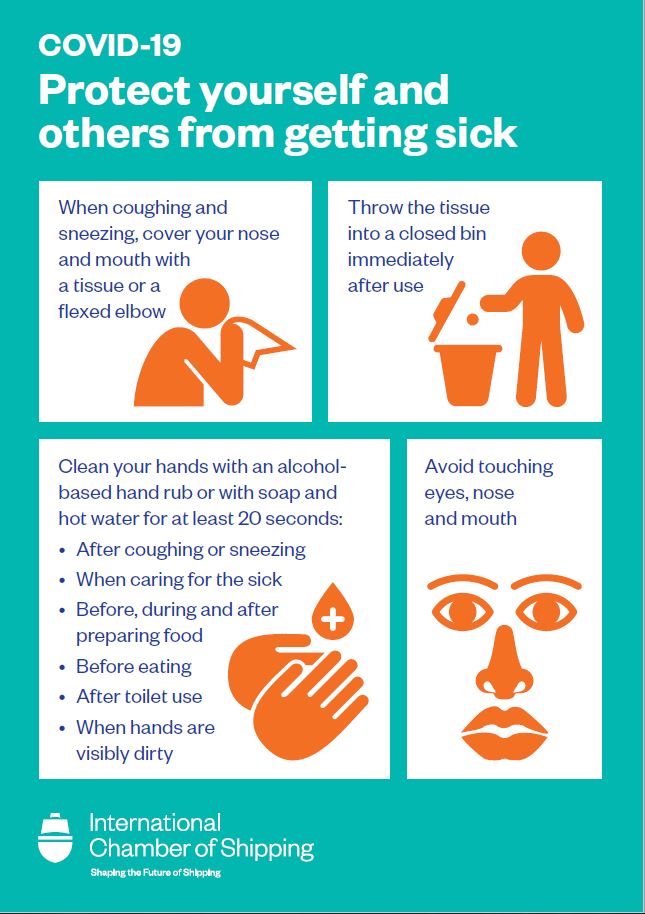
When someone infected with a respiratory disease, such as COVID-19, coughs or sneezes they project small droplets containing the virus. Sneezing or coughing into hands may contaminate objects, surfaces or people that are touched. Standard Infection Protection and Control (IPC) precautions emphasise the vital importance of hand and respiratory hygiene. In particular:
• Frequent hand washing by crew (and passengers) using soap and hot water or alcohol-based (at least 65–70%) hand rub for 20 seconds;
• Avoidance of touching the face including mouth, nose and eyes with unwashed hands (in case hands have touched surfaces contaminated with the virus);
• Seafarers (and passengers) should be encouraged to cover their nose and mouth with a disposable tissue when sneezing, coughing, wiping and blowing the nose then dispose of the used tissue immediately;
• If a tissue is not available, crew should cover their nose and mouth and cough or sneeze into a flexed elbow;
• All used tissues should be disposed of promptly into a waste bin;
• Seafarers should aim to keep at least one metre (3 feet) distance from other people, particularly those that cough or sneeze or may have a fever. If they are too close, other crew members can potentially breathe in the virus; and
• Meat, milk or animal products should always be handled with care, to avoid cross-contamination with uncooked foods, consistent with good food safety practices.
It is important that seafarers should be given the time and opportunity to clean their hands after coughing, sneezing, using tissues, or after possible contact with respiratory secretions or objects or surfaces that might be contaminated.
Although face masks may provide some protection – especially if there is a risk of exposure when interacting with persons from outside the ship – the routine use of face masks is not generally
recommended as protection against COVID-19. WHO advises that it is appropriate to use a mask when coughing or sneezing. If an individual is healthy, it is only necessary to wear a mask if the person is taking care of a person with the suspected COVID-19 infection.
www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/when-and-how-to-use-masks
Hand and respiratory hygiene are considered far more important.
Safety posters for ships are provided in Annex A.
4 Outbreak Management Plan for COVID-19
Ships should develop a written outbreak management plan. Seafarers on board should have knowledge of the outbreak management plan and implement it as required.
Passengers and Seafarers should receive information in accordance with the WHO advice for international traffic regarding the outbreak of COVID-19.
Advice is available on the WHO website for COVID-19 at www.who.int/health-topics/coronavirus
5 Pre-Boarding Information
This Guidance uses information contained in the WHO Operational considerations for managing COVID-19 cases/outbreak on board ships, interim guidance 24 February 2020. It is also recommended to use this alongside the WHO Handbook for Management of Public Health Events on Board Ships.
www.who.int/publications-detail/operational-considerations-for-managing-covid-19-cases-outbreak-onboard- ships
6 Pre-boarding Screening
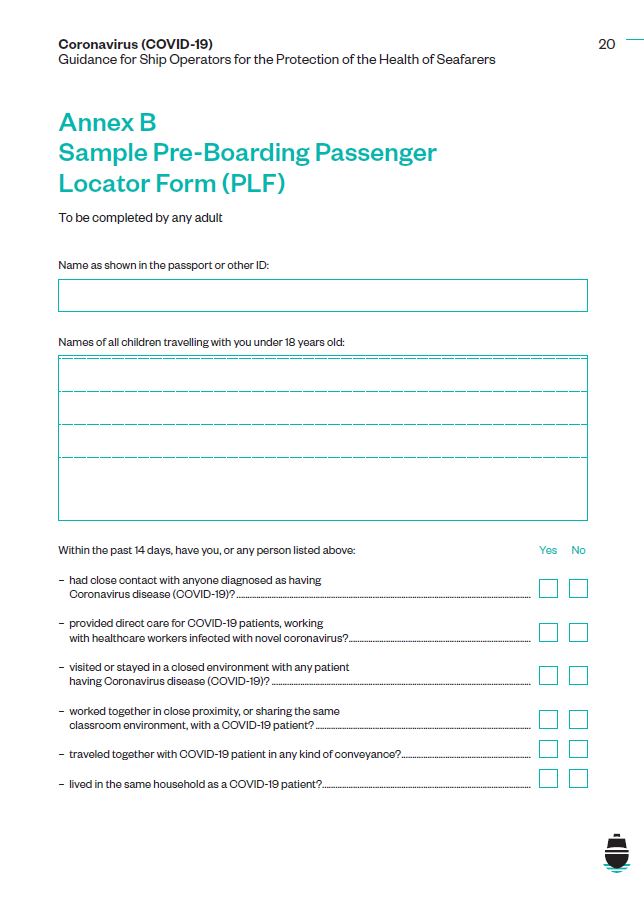
Until the end of the COVID-19 outbreak, all ships are advised to provide passengers and seafarers with general information on COVID-19 and its preventative measures and implement pre-boarding screening.
A sample pre-boarding Passenger Locator Form (PLF) is provided in Annex B. The purpose is to identify passengers who may need to have their boarding deferred or rescheduled and to ensure proper management by competent health authorities.
7 Information and Awareness
Ship Operators should provide guidance to crew on how to recognise the signs and symptoms of COVID-19. Crew should be reminded of the plan and procedures to follow if a passenger or crew member on board displays signs and symptoms of acute respiratory disease.
Country-specific guidance about prevention measures may be available, such as at www.cdc.gov/quarantine/maritime/recommendations-for-ships.html
Medical staff on board ships should be informed and updated about the outbreak of COVID-19 and any new evidence and guidance available. It is recommended to review the WHO website for COVID-19. Information about the use of medical masks can also be found on the website.
The posters provided at Annex A can also be used onboard to provide a gentle reminder of best practices for seafarers to adopt. They are also available for download from the ICS website at
www.ics-shipping.org/free-resources
8 Suspected Cases of Infection
If people only have mild respiratory symptoms and have not visited an area where COVID-19 has been reported within the past 14 days, or if they have been in close contact with someone with respiratory symptoms who has been to a place which has COVID-19, they should still carefully practise basic hand and respiratory hygiene and isolate themselves, if possible, until fit.
If the virus spreads more widely this definition may change, but a suspect case requiring diagnostic testing is generally considered to be:
A patient with acute respiratory illness (fever and at least one sign/symptom of respiratory disease (e.g. cough, shortness of breath), and with no other set of causes that fully explains the clinical presentation and a history of travel to or residence in a country/ area or territory reporting local transmission of (COVID-19) during the 14 days prior to the onset of the symptoms.
Or
A patient with any acute respiratory illness and having been in contact with a confirmed or suspected COVID-19 case during the 14 days prior to the onset of the symptoms.
Or
A patient with severe acute respiratory infection (fever and at least one sign/symptom of respiratory disease e.g. cough, shortness of breath and requiring hospitalization and with no other set of causes that fully explain the symptoms.
Any person on board that may have been in close contact with a suspect case should be:
• Traced immediately after the suspect case is identified;
• Asked to remain on board until laboratory results of the suspect case are available (measures that apply following positive laboratory results are described below); and
• Categorised as either contacts with high risk exposure or with low risk exposure.
Further guidance can be found at www.who.int/publications-detail/global-surveillance-for-human-infection-with-novel-coronavirus-(2019-ncov)
All persons on board that fulfil the definition of a ‘close contact’ (see below) should be asked to complete a PLF (see Annex B) and remain on board the ship in their cabins or preferably at a specially designated facility ashore (if feasible and in case that the ship is at the turnaround port where embarking/disembarking passengers or discharging/loading cargos/stores takes place), in accordance with instructions received by the competent health authorities, until the laboratory result for the suspect case is available. Persons on board who do not fulfil the definition of a ‘close contact’ will be considered as having low risk exposure and should:
• Be requested to complete PLFs with their contact details and the locations where they will be staying for the following 14 days;
• Be provided with the following information and advice on the details of symptoms and how the disease can be transmitted;
• Be asked to self-monitor for COVID-19 symptoms, including fever of any grade, cough or difficulty breathing, for 14 days from their last exposure; and
• Be asked to immediately self-isolate and contact health services in the event of any symptom appearing within 14 days. If no symptoms appear within 14 days of their last exposure, the contact person is no longer considered likely to develop COVID-19.
9 Close Contacts (High Risk Exposure)
A ‘close contact’ is a person who, for example:
• Has stayed in the same cabin with a suspect/confirmed COVID-19 case;
• Has had close contact within one metre or was in a closed environment with a suspect/confirmed COVID-19 case (for passengers this may include sharing a cabin);
• Participated in common activities on board or ashore;
• Participated in the same immediate travelling group;
• Dined at the same table (for crew members this may include working together in the same ship area);
• Is a cabin steward who cleaned the cabin;
• Is restaurant staff who delivered food to the cabin;
• Is a gym trainer who provided close instruction to a case; or
• Is a medical support worker or other person providing direct care for a COVID-19 suspect or confirmed case.
Close contacts may be difficult to define on board a confined space such as a passenger ship, and if widespread transmission is identified then all persons on board could be considered as ‘close contacts’ having had high risk exposure.
10 Hygiene Measures for Seafarers on Ships
Ship operators should provide specific guidance and training for their seafarers regarding:
• Hand washing (using soap and hot water, rubbing hands for at least 20 seconds; one way to know how long 20 seconds is would be to silently sing “happy birthday to you!” twice);
• When hand washing is essential (e.g. after assisting an ill traveller or after contact with surfaces they may have contaminated, etc);
• When to hand rub with an antiseptic instead of hand washing, and how to do this;
• How to cough and sneeze hygienically (e.g. using disposable tissues or a flexed elbow);
• Appropriate waste disposal;
• When and how to use masks; and
• Avoiding close contact with people suffering from acute respiratory infections.
11 Management of Suspect Cases by Medical Support Providers
If someone on board is suspected to have COVID-19, Personal Protective Equipment (PPE) for interview and assessment may be used by medical support providers.
Key outbreak control activities will include supportive treatment, e.g. giving oxygen, antibiotics, hydration and fever/pain relief.
12 Precautions at the Ship Medical Facility
The following precautions should be taken:
• Patients must cover their nose and mouth with a tissue when coughing or sneezing; or a flexed elbow if not wearing a mask. This should be followed by performing hand hygiene with an alcohol-based hand rub (at least 65–70%) or soap and hot water for 20 seconds.
• Careful hand washing should occur after contact with respiratory secretions.
• Suspect cases must wear a medical mask once identified and evaluated in a private room with the door closed, ideally an isolation room;
• Any person, including healthcare workers, entering the room should apply appropriate precautions in accordance with the requirements of WHO infection prevention and control during healthcare when COVID-19 is suspected; and
• After preliminary medical examination, if the ship’s medical officer or person responsible for the provision of medical care believes a suspect case exists, the patient should be isolated.
If the illness is not considered a suspect case but the person has respiratory symptoms, the person should still not return to any places where they will be in contact with others onboard either seafarers or passengers..
13 Laboratory Testing
Laboratory examination of clinical specimens for suspect cases should be made with the competent authorities at the port who will then inform the ship’s officers about test results.
14 Case Handling
Case handling should:
• Be initiated by the ship’s medical care providers in order to detect any new suspect cases;
• Include directly contacting crew and passengers, asking about current and recent illnesses, and checking if any person meets the criteria for a suspect case; and
• Be recorded in the appropriate medical log book.
Medical care providers should:
• Ensure a suspect case is interviewed and provide information about the places they have visited within the last 14 days prior to the onset of symptoms and their contacts, including the period from one day before the onset of symptoms on board the ship or ashore; and
• Keep records regarding:
– Anyone on board who has visited the medical facility as a suspect case and the isolation and hygiene measures taken;
– Any close contact or casual contact with low risk exposure to monitor their health;
– Contact details of casual contacts with low risk exposure who will disembark and the locations where they will be staying in the next 14 days (completed PLFs or Maritime Declarations of Health (MDHs); and
– Results of active surveillance.
15 Isolation
Isolate suspect cases on board immediately and inform the next port of call of suspect cases:
• With acute respiratory infection, either a cough, sore throat, shortness of breath, whether requiring hospitalisation or not;
• Who in the 14 days before onset of symptoms met the definition of a suspect case as outlined in sections 8 and 9.
Patients should be isolated in either an isolation ward, cabin, room or quarters with precautionary measures.
Anyone entering an isolation room should wear gloves, impermeable gowns, goggles and medical masks.
16 Reporting to the Next Port of Call
The competent authority of the next port of call must always be informed if there is a suspect case on board.
For ships on an international voyage, if someone has died on board the International Health Regulations (IHR) state that the MDH should be completed and sent to the competent authority in accordance with local requirements.
The Master should immediately alert the competent authority at the next port of call about any suspect case to determine if the necessary capacity to transport, isolate, and care for the individual is available.
The ship may need to proceed, at its own risk, to another nearby port if capacity is not available, or if warranted by the critical medical status of the suspect case.
After measures applied are considered by the port health authority to be completed satisfactorily, the ship should be allowed to continue the voyage. The measures taken should be recorded in the valid ship sanitation certificates. Both embarking and disembarking ports must be notified of contacts on board and any measures taken.
17 Disembarkation of a Suspect and a Confirmed Case
The ship should take the following precautions:
• Control disembarkation to avoid any contact with other persons on board;
• The patient should wear a surgical mask; and
• Personnel escorting the patient should wear suitable PPE (gloves, impermeable gown, goggles and medical mask).
The ship may proceed to its next port of call once the health authority has determined that public health measures have been completed satisfactorily in particular the measures as follows:
• Management of the suspect case or cases and close contacts;
• Completion of contact tracing forms, disembarkation of close contacts; until the termination of COVID-19 Public Health Emergency of International Concern is declared. All passengers and crew members should fill in a PLF to be kept on board for at least one month after disembarkation;
• Information in the completed PLF should be provided upon the request of health authorities to facilitate contact tracing if a confirmed case is detected after the disembarkation and after the voyage has ended;
• Information has been provided to everyone on board about the symptoms and signs of the disease and who to contact in case the relevant symptoms develop in the following 14 days; and
• Cleaning and disinfection, and disposal of infectious waste.
18 Cleaning, Disinfection and Waste Management
Maintain high level cleaning and disinfection measures during ongoing on board case management.
Patients and ‘close contacts’’ cabins and quarters should be cleaned and using cleaning and disinfection protocols for infected cabins (as per Norovirus or other communicable diseases).
Environmental surfaces should be cleaned thoroughly with hot water, detergent and applying common disinfectants (e.g. sodium hypochlorite).
Once a patient has left the ship, the isolation cabin or quarters should be thoroughly cleaned and disinfected by staff using PPE who are trained to clean surfaces contaminated with infectious agents.
Laundry, food service utensils and waste from cabins of suspect cases and contacts should be treated as infectious, in accordance with procedures for handling infectious materials on board.
There should be regular communications between departments in all ships (medical, housekeeping, laundry, room service, etc) about the persons in isolation.
19 Management of Contacts of a Suspect Case
Port health authorities will conduct risk assessments to identify all contacts, and issue instructions to follow until laboratory results are available.
All close contacts should either complete PLFs or MDHs and remain in their cabins or at a facility ashore and follow the competent authority’s instructions until laboratory results are available. The forms should contain contact details and locations where the suspect case will stay for the following 14 days.
All close contacts should be informed about the suspect case on board.
If the laboratory examination results are positive:
• All close contacts should be quarantined for 14 days; and
• The patient should disembark and be isolated ashore in accordance with the competent authority’s instructions.
Quarantine measures should follow WHO guidance of considerations for quarantine of individuals in the context of COVID-19 and are also likely to include:
• Active monitoring by the port health authorities for 14 days from last exposure;
• Daily monitoring (including fever of any grade, cough or difficulty breathing);
• Avoiding social contact and travel; and
• Remaining reachable for active monitoring.
Contacts of a confirmed case should immediately self-isolate and contact health services if symptoms appear within 14 days of last exposure. If no symptoms appear, the contact is not considered at risk.
Implementation of specific precautions may be modified following risk assessment of individual cases and advice from port health authorities.
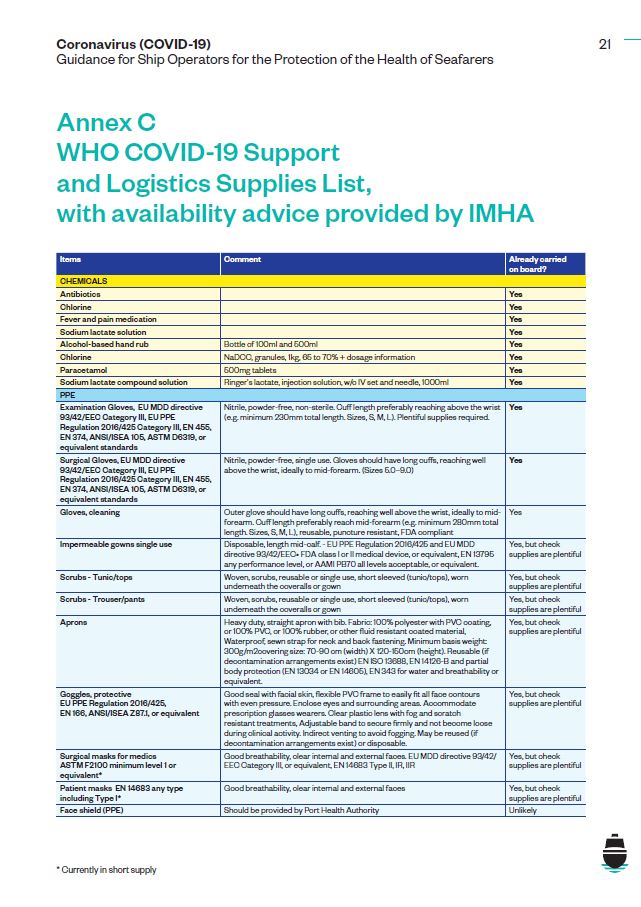
20 Supplies and Equipment
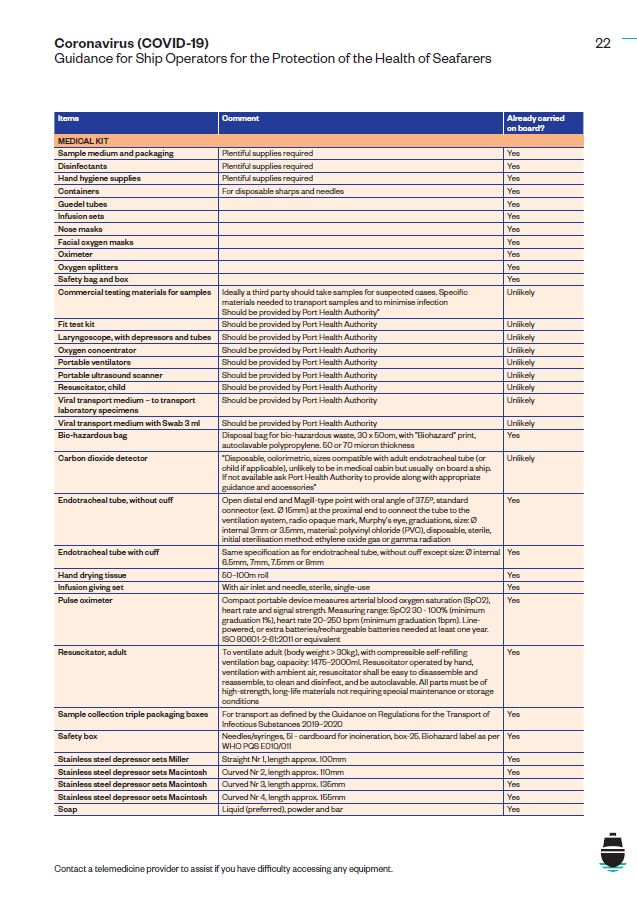
Flag States regulate medical supply carriage requirements. Plentiful supplies and equipment should be available to handle an outbreak as described in the International Medical Guide for Ships 3rd edition.
Reviewing the latest WHO suggested list of supplies for COVID 19, the International Maritime Health Association (IMHA) has advised that most equipment should already be on board. However, WHO also recommends other equipment that is unlikely to already be on board which IMHA suggest could be provided by a port health authority.
A table is attached at Annex C outlining the supplies and equipment required in a situation of COVID-19.
This is based on information provided by WHO and the IMHA.
www.who.int/publications-detail/disease-commodity-package—novel-coronavirus-(ncov)
Annex A
Posters
WHO and ECDC, among others, have provided advice to avoid the spread of COVID-19. To highlight their key messages and to help seafarers know how best to protect themselves and those they meet, ICS has produced the following three posters for ships.
The posters are also available to download from the ICS website at: http://www.ics-shipping.org/free-resources